Measure 001 requires documentation of the HbA1c level for diabetic patients between the ages of 18-75. This is an inverse measure – this means YOU DO NOT WANT TO MEET THIS MEASURE. The best score for this measure is a 0.
If the patient’s HbA1c is greater than 9.0%, you meet the measure. This level of HbA1c is outside the healthy range.
You must collect HbA1c levels for all patients that qualify for this measure to get a good score. Every diabetic patient between the ages of 18 and 75 that do not have their HbA1c documented counts against you.
The HbA1c level must come from a lab result, you cannot accept patient reported information.
The lab test can be:
- • From a test you ordered
- • From a test another doctor ordered
- • From the patients hospital, or nursing home chart.
When documenting the information please always be sure to document the source of the information. If you can get a copy of the lab report into the patients chart that is best.
As a telehealth provider, you can report on this measure. Get a copy of the lab result with the HbA1c level and include it as part of the patient’s chart.
The doctor does not need to be the one to collect the HbA1c level. A staff member can reach out to the patient’s primary care doctor or endocrinologist to have the report faxed over. The doctor’s responsibility is to review the level.
If there are multiple HbA1c tests performed, the most recent measurement will be the recorded level for this measure.
Exclusions
There are several reasons a patient may be excluded from this measure:
- • Patient is on hospice
- • Patient is on palliative care
- • Patient is 66 or older and in an Institutional Special Needs Plan
- • Patient is 66 or older with at least one encounter for frailty AND dispensed a medication for dementia
- • Patient is 66 or older with at least one encounter for frailty AND at least one acute inpatient admission with a diagnosis of an advanced illness
- • Patient is 66 or older with at least one encounter for frailty AND has had at least 2 visits to an ED or outpatient observation or non-acute inpatient encounters on different dates of service with an advanced illness diagnosis
If a patient falls under one of these exclusions, you must document why the patient is exempt to ensure the patient doesn’t count against you. Include the code and diagnosis in the patient’s medical problem list and the claim.
You can review the codes that qualify the patient to be excluded from the measure here (https://qpp.cms.gov/docs/QPP_quality_measure_specifications/CQM-Measures/2024_Measure_001_MIPSCQM.pdf)
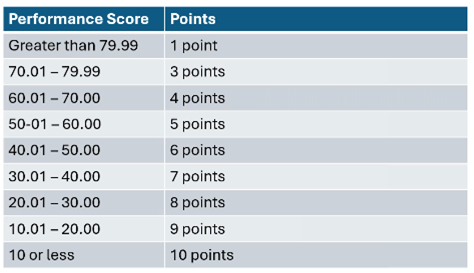
Our goal is to get 60/60 points in quality measures. You have to report on 6 measures. If you are a small practice, you get an additional 6 bonus points. By scoring an average of 9 on the six measures, and adding the 6 bonus points, you will score a perfect 60/60 in quality. This puts you in a good position to possibly earn a bonus at the end of the year for having a high composite MIPS score.
Contact Registry Clearinghouse at info@registryclearinghouse.com or schedule a meeting to learn more about how Registry Clearinghouse can help you.



Read Comments